Say Goodbye to Heel Pain: 7 Surprising Secrets to Cure Plantar Fasciitis
Persistent heel pain can be a significant challenge, making each step difficult.
This discomfort may indicate plantar fasciitis, a prevalent condition affecting many individuals, particularly those who lead active lifestyles or spend extended periods on their feet.
This article aims to provide an in-depth understanding of plantar fasciitis, including its causes, symptoms, and effective treatment options.
Additionally, we offer practical tips for prevention and guidance on when to seek medical assistance. Continue reading to learn how to restore comfort and mobility.
Last update on 2025-10-01 / Affiliate links / Images from Amazon Product Advertising API
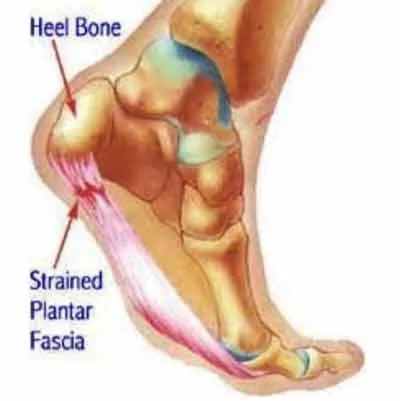
What is Plantar Fasciitis?
Plantar fasciitis is a prevalent foot condition marked by inflammation of the plantar fascia, a robust band of tissue that extends across the bottom of the foot, linking the heel bone to the toes.
This condition frequently leads to considerable heel pain, particularly noticeable during the initial steps taken in the morning or following extended periods of inactivity.
It can affect individuals across various age groups, especially those who are physically active or lead sedentary lifestyles.
It results in discomfort that can adversely impact daily activities and overall mobility. Understanding proper alignment and body mechanics can help mitigate this foot pain.
What Causes Plantar Fasciitis?
Plantar fasciitis can be attributed to various causes, including overuse injuries, improper foot alignment, and several risk factors, such as obesity or participation in high-impact activities.
Environmental factors and footwear choices also play a significant role in developing this condition.
This condition typically develops gradually due to repetitive strain on the plantar fascia, resulting in inflammation and pain, particularly in the heel region.
Incorporating appropriate stretching exercises and physical therapy can help manage these symptoms effectively.
Furthermore, inadequate footwear that provides insufficient arch support can exacerbate the condition, increasing strain and discomfort.
Custom orthotics and insoles may offer necessary support and aid in inflammation reduction.
1. Overuse or Repetitive Strain
Overuse or repetitive strain primarily contributes to plantar fasciitis, often impacting athletes and individuals engaged in high-impact activities such as running or jumping.
This strain exerts excessive stress on the plantar fascia, resulting in micro-tears and chronic inflammation.
Consequently, individuals may experience acute pain, particularly during activities involving prolonged standing or sudden movements.
In addition to running and jumping, other activities such as dancing, aerobics, or extended periods of walking on hard surfaces can further increase the risk of developing this condition.
When individuals exceed their physical limits without sufficient rest, the cumulative effect of these repetitive motions may lead to significant discomfort.
Rehabilitation techniques such as stretching and strength training, which can alleviate tension in the affected area, are essential to effectively managing this pain.
Furthermore, ensuring adequate rest and allowing the body sufficient time to recover can substantially enhance the healing process, prevent the recurrence of injuries, and promote overall foot health.
2. High-impact Activities
Engaging in high-impact activities such as running, dancing, or playing sports considerably increases the risk of developing plantar fasciitis due to the stress placed on the heel and foot arch.
These activities can result in heel pain, particularly when performed without proper warm-up or when unsuitable footwear is worn that lacks adequate shock absorption and arch support.
It is essential to manage the intensity and frequency of these activities to prevent this condition.
To minimize discomfort and promote foot health, individuals should prioritize selecting appropriate footwear designed for their activity type, ensuring that the shoes fit well and provide adequate cushioning.
Exploring therapeutic modalities such as ice and massage therapy can also benefit.
Incorporating a consistent warm-up routine that includes stretching and strengthening exercises for the calves and arches can prepare the feet for the demands of high-impact movements.
By implementing effective pain management techniques and sound foot care strategies, individuals can significantly reduce the likelihood of developing plantar fasciitis, enhancing overall performance and enjoyment in their chosen sports.
3. Improper Footwear
Improper footwear is a significant contributing factor to the development of plantar fasciitis, as shoes that lack sufficient arch support and cushioning can result in misalignment and increased strain on the plantar fascia.
This support deficiency can exacerbate pain and inflammation, particularly in individuals with flat feet or high arches, thus highlighting the importance of selecting footwear that supports the foot’s structural integrity.
Many common types of footwear, including flip-flops, ballet flats, and high heels, often fail to deliver the necessary arch support and cushioning required to protect the feet.
Consequently, these styles can aggravate existing pain or contribute to the onset of plantar fasciitis in individuals predisposed to this condition.
Supportive footwear designed with contoured footbeds, shock-absorbing soles, and reinforced arches can significantly alleviate discomfort. Investing in high-quality athletic shoes or orthotic inserts promotes proper alignment and reduces stress on the plantar fascia, ultimately enhancing foot health and providing pain relief.
4. Obesity
Obesity is a significant risk factor for plantar fasciitis, as excess body weight increases the strain on the plantar fascia, resulting in inflammation and heel pain.
The additional stress can exacerbate pre-existing conditions and impede recovery time, making weight management a crucial element in both the prevention and treatment of this condition.
Individuals experiencing obesity may find that losing excess weight can greatly alleviate their symptoms.
This weight reduction diminishes the pressure on the feet, facilitating improved foot anatomy and function.
Achieving a healthy body weight alleviates discomfort and reduces the risk of future foot-related complications.
Implementing weight management strategies, such as regular physical activity and a balanced diet, can significantly enhance overall foot health.
This proactive approach offers lasting benefits, improving mobility and ensuring a higher quality of life for those affected by this painful condition.
- ✶REDUCES HEEL & FOOT PAIN – Using the ProStretch daily reduces pain and inflammation caused by plantar fasciitis, Achilles tendonitis, Sever’s disease, shin splints, and tight calves / hamstrings. The ProStretch calf stretcher isolates the lower leg muscles, tendons, and ligaments to ensure a deep, effective stretch that helps to reduce injuries.
- ✶PHYSICIAN TRUSTED & APMA ACCEPTED – This foot rocker is medically proven to be effective and found in physical therapy clinics worldwide. The gentle motion of the ProStretch provides a deeper and more effective stretch than conventional methods.
- ✶SLIP-RESISTANT PADS – The advanced rubber strips on the bottom of the ProStretch protect against moving and sliding, allowing for a safe and effective stretch. The slip-resistant pads ensure that the calf stretcher does not slide when used on any surface.
- ✶PROVEN EFFECTIVE DESIGN – The unique rocker design holds the foot in the optimal position for an accurate and efficient stretch, increasing flexibility and enhancing overall performance.
- ✶NOTES ON USE – Fits adult shoes up to size 12. The recommended weight limit is 250 lbs. Wear socks and athletic shoes while using the ProStretch.
Last update on 2025-10-01 / Affiliate links / Images from Amazon Product Advertising API
What Are the Symptoms of Plantar Fasciitis?
The symptoms of plantar fasciitis generally manifest as persistent heel pain, often described as sharp or stabbing sensations experienced upon taking the first steps in the morning or after prolonged periods of inactivity.
Additionally, many individuals report stiffness and tenderness along the bottom of the foot, which may impede walking and cause significant discomfort.
Engaging in yoga and flexibility exercises can enhance mobility and alleviate symptoms.
Early recognition of these symptoms is crucial for implementing effective interventions and managing pain appropriately.
1. Heel Pain
Heel pain is the primary symptom associated with plantar fasciitis, commonly described as a sharp or burning sensation that typically intensifies after periods of rest.
This pain can significantly disrupt activities such as walking, running, or even standing, making it essential for individuals experiencing this symptom to seek appropriate pain assessment and management strategies.
The discomfort often escalates in intensity with prolonged activity, profoundly affecting daily functioning and overall quality of life.
Patients frequently report that the pain is most severe during the initial steps in the morning or following extended periods of immobility.
Pain assessment tools can provide valuable insights into the specific characteristics of the discomfort, while integrating practical foot exercises may offer considerable relief.
Examples of beneficial exercises include:
- Stretching the calf muscles
- Performing toe curls
Both of which can alleviate tension and promote healing. Understanding and addressing these factors is crucial for successful recovery.
2. Stiffness and Tenderness
Patients diagnosed with plantar fasciitis frequently report experiencing stiffness and tenderness along the arch and heel of the foot, particularly following extended periods of inactivity, such as during sleep or prolonged sitting.
This stiffness can lead to a restricted range of motion and discomfort during the initial steps taken upon waking or after sitting, thereby underscoring the necessity for effective pain relief strategies.
Addressing this discomfort typically involves a multifaceted approach incorporating targeted pain relief techniques to enhance flexibility and alleviate tension in the affected areas.
Stretching exercises, for example, are essential in mitigating tightness and improving circulation, which can ultimately reduce the sensation of stiffness.
Additionally, soft tissue therapy can offer considerable benefits by concentrating on releasing muscle and fascia, thereby facilitating improved mobility and diminishing tenderness.
Collectively, these strategies help manage pain effectively and empower individuals to regain control over their daily activities without the burden of ongoing foot discomfort.
3. Difficulty in Walking
Difficulty walking is a prevalent concern for individuals affected by plantar fasciitis, as heel pain and discomfort can disrupt standard gait patterns and overall mobility.
Many individuals may find themselves avoiding certain activities or modifying their walking style to alleviate pain, which underscores the significance of self-care and therapeutic exercises in effectively managing this condition.
Many experience sharp pain with each step, which often results in a cycle of reduced activity levels, which can further weaken the foot’s support structures and exacerbate symptoms.
Engaging in gentle stretching routines, strengthening the muscles of the feet and legs, and utilizing supportive footwear are essential practices for recovery.
Incorporating specific rehabilitation techniques, such as physical therapy, can provide targeted relief and enhance flexibility, ultimately improving functionality.
By prioritizing these methods, individuals can regain their mobility, enabling them to return to daily activities with increased confidence and reduced discomfort.

What Are the Medical Treatment Options for Plantar Fasciitis?
Treatment options for plantar fasciitis encompass a spectrum of approaches, ranging from conservative methods, such as rest, ice therapy, and stretching exercises, to more advanced interventions, including physical therapy and corticosteroid injections.
These methods are designed to alleviate chronic pain, reduce inflammation, and facilitate recovery, enabling individuals to resume their daily activities and maintain an active lifestyle.
A comprehensive approach that integrates multiple strategies typically produces the most effective outcomes for managing this condition.
1. Rest and Ice Therapy for Heel Spur Relief
Rest and ice therapy are essential components of the treatment plan for plantar fasciitis, including heel spurs, as they significantly reduce inflammation and provide necessary pain relief.
Refraining from activities exacerbating heel pain and applying ice to the affected area can markedly improve symptoms and facilitate healing.
To implement these techniques effectively, it is crucial to rest the foot, allowing the inflamed tissues to recover without undue stress.
Experts recommend icing the affected area for approximately 15 to 20 minutes several times daily, particularly following any activities that may aggravate the condition.
This method alleviates pain and constricts blood vessels, reducing swelling and promoting a quicker recovery.
These strategies are integral to a comprehensive pain management approach.
They complement other treatments, such as stretching and strengthening exercises, enhancing mobility and comfort.
2. Stretching and Strengthening Exercises for Injury Prevention
Incorporating stretching and strengthening exercises into a treatment regimen is essential for managing plantar fasciitis.
These therapeutic exercises enhance flexibility and support recovery by addressing muscle tension and imbalances.
Targeted stretching routines for the Achilles tendon and plantar fascia can alleviate pain, while strengthening exercises improve foot stability and alignment.
For effective pain management, performing these exercises consistently, ideally five to six days weekly, is advisable.
Stretching may include holding calf stretches for 15 to 30 seconds, targeting at least three repetitions for each foot.
This approach not only aids in elongating the tissues but also promotes blood flow to the affected area.
Strengthening exercises, such as toe curls and marble pickups, should be incorporated to enhance the foot’s intrinsic muscles, thereby contributing to improved overall foot mechanics.
Committing to a balanced exercise program that includes stretching and strengthening activities is crucial for stabilizing the foot and minimizing discomfort, ultimately making daily activities more manageable.
3. Orthotic Devices and Night Splints
Orthotic devices, including custom orthotics and heel cushions, are essential in managing plantar fasciitis.
They provide critical arch support and pain relief.
These devices enhance foot alignment, evenly distribute weight, and minimize strain on the plantar fascia, facilitating recovery and improving comfort during daily activities.
In addition to custom orthotics, which are meticulously designed to conform to an individual’s foot’s unique contours, over-the-counter alternatives, such as arch supports and gel insoles, can provide significant relief.
The functionality of these assistive devices varies depending on the severity of the condition, ranging from stabilizing the arch to offering additional cushioning.
By ensuring adequate arch support, orthotic devices alleviate excessive pressure on the plantar fascia, promote healing, and enable individuals to resume everyday routines.
Ultimately, the appropriate use of orthotic devices can improve long-term outcomes for individuals with this painful foot condition.
4. Physical Therapy and Ultrasound Therapy
Physical therapy is a highly effective treatment option for individuals suffering from plantar fasciitis, incorporating a variety of therapeutic modalities aimed at alleviating pain, enhancing flexibility, and restoring functionality.
Physical therapists may utilize ultrasound, massage, and joint mobilization techniques to address muscle tension and promote healing in the affected region.
Personalized exercise programs that focus on strengthening the foot and calf muscles are essential to rehabilitation, as they contribute to improved overall stability and mobility.
Stretching exercises are frequently integrated to enhance the ankle’s range of motion and reduce tension in the plantar fascia.
Additionally, therapeutic modalities like electrical stimulation may improve circulation and assist pain management.
The recovery process emphasizes education regarding appropriate footwear and gait mechanics, promoting long-term relief and functional improvement.
Through a comprehensive approach, physical therapy aims to equip patients with the necessary tools to manage and overcome their condition effectively.
5. Medications and Topical Treatments
Medications are critical in managing the pain and inflammation associated with plantar fasciitis.
Treatment options range from over-the-counter anti-inflammatory medications to corticosteroid injections for more severe cases.
These interventions can reduce swelling and alleviate pain, enabling individuals to engage in rehabilitation and therapeutic exercises.
In addition to these conventional options, some individuals may benefit from topical treatments that provide localized relief and oral pain relievers that assist in managing discomfort throughout the day.
It is essential for those experiencing plantar fasciitis to consider these medications as part of a comprehensive pain management strategy, which should also include physical therapy, stretching, and the use of supportive footwear.
Addressing the symptoms and the underlying causes of the condition can make recovery more efficient, facilitating a return to normal activities once inflammation subsides and mobility improves.
- Immediately relieves plantar fasciitis heel pain from plantar fasciitis & heel spurs treating pain directly at the source. Prevents plantar fasciitis from coming back.
- Distributes foot pressure evenly across the foot, reducing pressure from the forefoot to the heel as you walk.
- Shock-absorbing deep heel cup manages heel inflammation, reduces stress and provides both cushioning and stability to the foot. Arch support hugs your foot in just the right spot to stop the plantar fascia from overstretching. Provides support across arch types, including high arches.
- Reduces morning plantar fasciitis pain.
- Full-length insole that can be easily trimmed to fit your shoe size.
Last update on 2025-09-30 / Affiliate links / Images from Amazon Product Advertising API
6. Injections and Acupuncture
In severe cases of plantar fasciitis where other treatments have proven ineffective, injection therapies, particularly corticosteroid injections, can offer significant pain relief and reduce inflammation.
These injections deliver anti-inflammatory medication directly to the affected area, facilitating rapid symptom relief and enabling a more focused rehabilitation approach.
Injections may be especially advantageous when conservative treatments, such as physical therapy or orthotics, do not produce satisfactory outcomes.
This method should be considered only after thoroughly assessing the patient’s condition and the severity of the pain experienced.
While the benefits frequently include a notable decrease in discomfort and an improved pathway to mobility, it is essential to recognize potential risks, including infection or tissue damage at the injection site.
Consequently, patients should discuss comprehensively with their healthcare provider to determine the most appropriate timing and frequency of injections within their overall pain management strategy.
7. Shockwave Therapy and Surgery
Shockwave therapy represents a cutting-edge treatment option for plantar fasciitis. It employs high-energy sound waves to promote healing and alleviate pain in the affected region.
This noninvasive technique has gained considerable traction due to its effectiveness in facilitating tissue regeneration and relieving pain.
It is positioning itself as an appealing alternative for individuals exploring options beyond traditional therapies.
By delivering targeted acoustic waves to the specific site of pain, this therapy enhances blood circulation, potentially accelerating the healing process.
Many patients report a significant reduction in discomfort after just a few sessions, underscoring its importance as a key component of a comprehensive pain management strategy.
The incorporation of shockwave therapy has the potential to improve mobility and overall function, enabling individuals to resume their daily activities with increased ease.
As more practitioners acknowledge its advantages, it may become essential in promoting long-term recovery and alleviating the challenges associated with chronic foot pain.
How to Prevent Plantar Fasciitis?
Preventing plantar fasciitis requires a comprehensive approach that includes appropriate footwear, regular stretching exercises, and maintaining a healthy weight.
By proactively addressing foot care and implementing lifestyle modifications, including wearing supportive running shoes, individuals can significantly reduce the risk of developing this painful condition and uphold an active lifestyle without discomfort.
1. Wear Proper Footwear and Running Shoes
Wearing appropriate footwear is essential for preventing plantar fasciitis, as shoes that offer adequate arch support and cushioning can significantly alleviate stress on the plantar fascia.
Footwear recommendations that consider ergonomic design can improve posture and joint health.
Selecting supportive footwear tailored to individual foot anatomy is critical for maintaining proper alignment and preventing the onset of heel pain.
The key characteristics of suitable shoes include:
- A firm heel counter that stabilizes the rearfoot,
- Comfortable cushioning that effectively absorbs shock,
- A contoured footbed that supports the arch and aids in biomechanical alignment.
Furthermore, proper shoe width prevents the foot from feeling cramped, promotes better circulation, and supports healthy biomechanics.
Individuals should also consider opting for a slightly elevated heel, which can help distribute weight evenly and support the foot’s natural positioning.
By investing time in selecting footwear that meets these criteria, individuals can enhance overall foot health and significantly reduce the risk of developing discomfort associated with this common condition.
2. Stretch Before and After Exercise
Incorporating stretching exercises before and after physical activity is critical for preventing plantar fasciitis.
It aids in maintaining flexibility in the plantar fascia and the surrounding musculature, which is part of effective therapeutic techniques.
An appropriate warm-up routine can significantly reduce the risk of overuse injuries and contribute to overall foot health.
To enhance this protective effect further, individuals may employ specific stretching techniques targeting the feet and lower legs, incorporating activity modification strategies.
Calf stretches are particularly advantageous, as they alleviate tension in the gastrocnemius and soleus muscles, thereby reducing strain on the heel and arch of the foot.
Additionally, toe stretches can improve the flexibility and strength of the intrinsic foot muscles, facilitating better balance during sports activities.
Incorporating ankle circles and resistance bands in stretching routines can promote mobility and help prevent conditions such as plantar fasciitis.
These targeted stretches enhance athletic performance and play a crucial role in long-term injury prevention, making them an essential component of any comprehensive exercise regimen.
3. Maintain a Healthy Weight
Maintaining a healthy weight is essential for preventing plantar fasciitis, as excess body weight places additional stress on the plantar fascia, thereby increasing the risk of inflammation and heel pain.
Adopting a holistic approach through lifestyle changes can enhance symptom management.
Implementing effective weight management strategies can contribute to overall foot health and decrease the likelihood of developing this condition.
Achieving and maintaining a healthy weight can significantly enhance mobility and reduce the strain on joints, particularly the feet.
For individuals experiencing obesity, it is imperative to incorporate regular physical activity alongside a balanced diet to alleviate the pressure placed on the plantar fascia.
Simple lifestyle modifications like walking or swimming can improve endurance while promoting weight loss.
When integrated into a comprehensive fitness routine, these endeavors can be further facilitated by consulting healthcare professionals for personalized nutrition plans.
By prioritizing weight management, individuals promote improved foot health and enhance their overall quality of life, ultimately reducing the risk of conditions such as plantar fasciitis through effective wellness strategies.
4. Rest and Listen to Your Body
Rest and active listening to one’s body are critical preventive measures for plantar fasciitis; neglecting symptoms may result in chronic pain and prolonged recovery times.
Understanding personal pain thresholds can aid in activity moderation.
Taking breaks during activities that impose excessive strain on the feet can help mitigate the risk of developing this painful condition.
Recognizing the early signs of discomfort is essential for maintaining optimal foot health.
It facilitates timely intervention before the situation escalates, involving professional guidance when needed.
Implementing structured rest periods in daily routines can significantly enhance recovery, allowing the body to repair and strengthen itself.
When individuals adopt a proactive approach regarding their physical limits, they improve their enjoyment of activities and promote long-term wellness.
Prioritizing rest reinforces the balance between activity and recovery, ultimately contributing to the overall health and resilience of the feet.
When should you seek medical help for plantar fasciitis?
When experiencing persistent heel pain that disrupts daily activities, seeking medical assistance for plantar fasciitis is essential.
Early intervention can facilitate more effective treatment options.
Consulting a podiatrist or foot specialist can provide valuable insights into diagnosis and customized management strategies for this prevalent foot condition.
Individuals should remain attentive to symptoms such as stiffness, swelling, and tenderness around the heel, particularly following periods of inactivity or extended standing.
Recognizing these signs promptly is crucial, as delaying treatment may lead to chronic pain and reduced mobility.
Healthcare professionals play a vital role in assessing the severity of the condition, recommending appropriate treatments such as physical therapy, orthotic devices, or corticosteroid injections, and guiding patients toward necessary lifestyle modifications and treatment protocols.
Professional advice assists in alleviating symptoms and preventing future recurrences, ensuring that individuals can restore their optimal function and return to their preferred activities confidently while following health strategies.
- Targeted Ankle Foot Pain Relief: This specially designed of Comfytemp ankle ice pack wrap is contoured to fit the ankle and foot region perfectly, ensuring maximum effectiveness in relieving ankle pains caused by swelling, sprains, bruises, inflammation, and arthritis. These reusable ice packs for ankle injuries provide active pain alleviation for a range of conditions, including plantar fasciitis, achilles tendonitis, gout pain, heel spur, sprained ankles, postoperative recovery, etc.
- Upgraded One-Piece Design: Comfytemp’s new ankle ice pack features an upgraded all-in-one design for easy use without additional accessories. The ice pack comes with 2 wide straps to securely wrap around your ankles, perfectly adapts to the curves of your feet, providing extra compression and a deeper, more intense cooling experience. This ankle ice pack Fits 7.5″-10″ ankle girth and Fits 7.5″-11″ arch girth. Tips: The ice pack does not cover the heel.
- Expert-grade Gel for Colder and Longer: Comfytemp ice pack for ankle pain filled with expert-grade gel, allowing the foot ice pack stays smooth and pliable even when frozen, ensuring a deeper and longer-lasting cold therapy, and allowing you to go about your daily activities. From athletes chasing peak recovery, to elderly individuals easing daily discomfort, to post-surgery patients seeking gentle support—Comfytemp delivers cold therapy that goes further, ensuring comfort at every step.
- Convenient, Cost-effective, Ever-ready, Alleviating: Contains 2 ankle ice packs. Offering convenient use on both ankles for long-term or recurring foot pain. With 2 ice packs, you can keep one in the freezer while using the other on sore muscles or injuries. It’s obviously cost-effective to buy both together, and having an extra ice pack on hand is handy for unexpected injuries. Experience the convenience, affordability, and preparedness of the Comfytemp ice pack set of 2 for ankle pain relief.
- Use It With Confidence: Features strong double edge and firm sewing ensures leak-proof performance and preventing any messy situations. With fully stickable outer layer and silky colder nylon inner, our product is built to last, ensuring long-term pain relief with its exceptional durability & reusability. More even gel makes consistent cold therapy & maximizes the cold pack effectiveness. This is a comprehensive solution for relieving ankle pain and promoting recovery.
Last update on 2025-10-01 / Affiliate links / Images from Amazon Product Advertising API
Frequently Asked Questions
What is plantar fasciitis, and how do I know if I have it?
Plantar fasciitis is a common condition that causes pain in the heel and bottom of the foot. It is often influenced by gait analysis and anatomical structures. Plantar fasciitis is caused by inflammation of the plantar fascia, a thick band of tissue that connects the heel bone to the toes. Symptoms include pain and stiffness in the heel and arch of the foot, especially in the morning or after prolonged rest periods.
How can I treat plantar fasciitis at home?
Several ways to treat plantar fasciitis at home include stretching exercises, icing the affected area, using over-the-counter pain relievers, and home remedies like essential oils. It’s also important to wear supportive shoes and avoid activities that strain the foot, such as running or standing for long periods.
When should I see a doctor for plantar fasciitis?
If your symptoms do not improve after a few weeks of at-home treatment, if the pain is severe, or if you experience difficulty walking or standing, you should see a doctor. Your doctor may recommend additional treatments, such as physical therapy or custom orthotics.
Can plantar fasciitis be prevented?
While plantar fasciitis is not always preventable, you can take steps to reduce your risk. These include wearing supportive shoes, maintaining a healthy weight, and avoiding high-impact activities that strain the feet.
How long does it take to heal from plantar fasciitis?
The healing time for plantar fasciitis can vary depending on the condition’s severity and the treatment’s effectiveness. In most cases, symptoms can take a few weeks to several months to fully subside.
Are there any long-term complications from plantar fasciitis?
If left untreated, plantar fasciitis can lead to chronic heel pain and difficulty walking or standing, potentially developing into chronic conditions. It’s essential to seek treatment immediately to prevent long-term complications.